- Home
- Past Conferences
- Exosomes in Human Infectious Diseases Conference
Exosomes in Human Infectious Diseases Conference
#EHID20
05 Mar - 08 Mar 2020
Nassau, Bahamas
Early Bird - Expired • Talk Submission - Expired • Poster Submission - Expired • Registration & Payment Deadline - Expired
Report
Extracellular vesicles (EVs), which are generated by almost all living cells, are now considered to be an important system of cell–cell communication. A large volume of data has been published on EVs in different fields of biology and medicine, from immunology to marine biology. The Exosomes in Human Infectious Diseases conference, hosted by Fusion Conferences, took place in The Bahamas from March 5 to March 8, 2020. The meeting focused on one of the most important aspects of EVs, their role in human infectious diseases.
The conference attracted attention of the EV experts from several different countries including the USA, France, Germany, Belgium, Canada, Portugal, Spain, Sweden, and Lebanon.
Attendees presented their recently obtained data over 4 days and engaged in lengthily fruitful discussions on the role of EVs in various human diseases. In a short report on the conference, it is impossible to describe all the important contributions. Below are presentations of some of the key findings. For a more complete and comprehensive list of topics and speakers, please refer to the conference programme.
In their introductory set of remarks, Co-Chairs of the Conference Drs. Fatah Kashanchi (George Mason University) and Leonid Margolis (NIH) emphasized the important role of small meetings that allow close interactions between scientists both at the sessions and during the free time. Such conferences are important for the progress in the field and for formulating its challenges. The immediate challenge is to distinguish the roles of various EVs that differ in size, composition and biogenesis in human infectious disease.
Dr. Clotilde Théry and her colleagues from the Institute Curie in Paris developed several technologies to separate EVs by size and analyze their composition. With advanced statistical analysis, they have developed an un-biased proteomic profiling approach to identify novel specific markers of the virus or sEV subtypes released by a human T lymphoma cell line. An interactive database defines groups of proteins with similar profiles, suggesting their release in the same class of EVs. Using this technique, the authors identified different categories of EVs, which bear different surface proteins in the context of HIV infection. In particular, the authors identified two cell-derived proteins that are included in the viral particles and one that is specific to non-viral sEVs that are modified by infection
The role of EV in viral infection in particular of HIV-1 was the focus of several other presentations. The importance of cargo molecules that EVs carry was emphasized in a Keynote presentation of Dr. Yoel Sadovsky (University of Pittsburgh). He focused on placenta that plays a critical role in maternal-fetal communication. The discovery of regulated trafficking of extracellular vesicles (EVs) has added a new dimension to our understanding of local and distant placental-maternal-fetal communication. He and his colleagues found that primary human placental trophoblasts, which form the front line of the maternal fetal interface, are resistant to infection by diverse types of viruses, in particular HIV-1. This resistance can be partly conferred to non-trophoblastic cells by transferring EVs contain C19MC miRNAs. The current work of this group centers on the mechanisms of uptake of trophoblastic exosomes by non-trophoblastic cells, where they found that macropinocytosis and clathrin-mediated endocytosis play a key role. The newly discovered pathways constitutes a defense mechanism against viral pathogens and possibly have other homeostatic functions during pregnancy.
Dr. Michael Bukrinsky (GWU School of Medicine and Health Sciences) presented data that showed impairment of cellular cholesterol metabolism in uninfected cells by Nef-containing extracellular vesicles (exNef). This may be a common factor driving pathogenesis of HIV-associated co-morbidities. He presented evidence for the role of exNef in reducing the abundance of ABCA1, inhibiting cholesterol efflux, upregulating lipid rafts, inducing inflammatory responses, and affecting neuronal myelination. He also discussed the potential implications for therapeutic approaches.
Dr. Fatah Kashanchi (George Mason University) discussed how viral EVs from 6 RNA viruses including HIV-1, HTLV-1, Rift Valley Fever, Zika, and Ebola among others were able to cause damage in the recipient cells. The EVs contained viral body parts including non-coding RNAs, viral proteins (from immediate early regions), and structural proteins needed for packaging. The mechanism of this de regulation was associated with autophagy and it intersects with EV release. He also discussed on EVs were released first from infected cells prior to virus release, making the recipient uninfected cells venerable to subsequent infection by an incoming virus.
EVs that affect HIV infection may be generated not only by the host cells, but also by microbiota. That was demonstrated in a presentation by Dr. Rogers Palomino from laboratory of Dr. Margolis (NICHD/NIH). In their work, they investigated the protective effect of vaginal Lactobacilli on transmission of HIV-1. They found that these bacteria release EVs that change viral Env in a way that inhibit HIV-1 infectivity in cell lines and in service-vaginal tissues ex vivo. Dr. Ramin Hakami (George Mason University) discussed the role of host exosomes during infection, using two model organisms; Yersinia pestis (Yp), and Burkholderia pseudomallei (Bp) surrogate species B. thailandensis (Bt). He indicated that Yp and Bp cause the emerging human diseases plague and melioidosis respectively and that there are no licensed vaccines or highly effective therapeutics are available for either of these diseases. His lab found that exosomes released from either Yp- or Bt-infected cells (designated as EXi) make naïve recipient cells strongly refractory to infection. In both cases, EXi caused differentiation of naïve human monocytes to macrophages and elicit strong release of specific proinflammatory cytokines that in turn induce increased bacterial clearance when the bacteria are encountered. Specific host signaling molecules were strongly modulated by the EXi, including p38, Jak2 and ALK, suggesting that a mechanistic model where the EXi protect the host by priming distant naïve monocytes to mount immune responses that improve resistance against infection.
Another interesting presentation was on picornaviruses presented by Dr. Esther Nolte-‘t Hoen (Utrecht University). She presented data on the packaging of non-enveloped (naked) viruses in EV. Her group studies viruses belonging to the picornaviridae family, which comprises many human and animal pathogens. For these viruses, the EV provide a host-derived membrane around the secreted virus particles, which can alter virus-host interactions. Using Encephalomyocarditis virus (EMCV), they recently showed that virus infection induced the timed release of multiple EV subsets. These EV subsets differ in biogenesis routes, packaging of virions and host molecules, and potential to spread infection. In her presentation, Nolte-‘t Hoen showed data of a follow-up study in which the role of viral and host factors in EV-mediated release of viruses was addressed. Hereto, they quantified and characterized EV produced during the infection with wild-type and mutant viruses using high-resolution flow cytometry, western blot analysis, and end-point titration. Their data supports a role for secretory autophagy in the release of EV-enclosed virus particles and implicates that specific viral security proteins play a role in this process. In addition, EVs are involved in herpes virus infection as evidenced by the results of Dr. Maria Kalamvoki from the University of Kansas Medical Center. She demonstrated that herpes simplex virus 1 (HSV-1) infection influences the cargo and functions of EVs released by infected cells and negatively affects HSV-1 infection through activation of antiviral responses. The team separated EVs that were positive for the tetraspanin CD63, from EVs that were positive for components of the endosomal sorting complexes required for transport (ESCRT) machinery. Functional characterization of these vesicles demonstrated that they have opposite effects on HSV-1 infection, but the dominant effect seems to be negative. Overall, they identified the dominant population of EVs, and other sub-populations produced during HSV-1 infection and have indications about their potential functions.
An important breakthrough in visualization of EVs was described by Dr. Guillaume van Niel (French Institute of Health and Medical Research). Together with Frederik Verweij in the group of Prof DM Pegtel (UMC, Amsterdam) they developed exosome optical reporters (including CD63-pHluorin) that detect exosome secretion using live-microscopy. They transferred this CD63-pHluorin tool to a zebrafish model to generate a suitable vertebrate model to follow exosomes them from their site of production to their final destination, using a combination of live-microscopy, electron microscopy techniques and proteomic ex vivo analysis. They studied exosome biogenesis, transfer, capture, uptake and fate at single-vesicle scale while retaining the in toto imaging scale of a compact vertebrate model system. The result of this study supported an unanticipated role for exosomes in nutrient delivery. This was the first model to study single EV release, transfer and function, combining in vivo imaging with sub-cellular of “clearance” mechanisms. With these new live-approaches, it has now become possible to open this “black-box” of exosomes dynamic and to live-track intercellular communication mediated by exosomes in vivo.
There was also an entire session devoted to ZIKA virus infection and EVs. Data from Dr. Schols’ group (from Rega Institute for Medical Research, KU Leuven, Belgium) was presented by Antonios Fikatas. They isolated ZIKV-infected human brain microvascular endothelial cell-derived EVs. Transwell-array system showed that these EVs were able to cross endothelial cells and further infect other brain-related cells (U87-glioblastoma). They identified two lactosylceramides and one phosphatidylserine that could be used as potential biomarkers. Dr. Jan Munch of the University Ulm (Germany) and his associates presented interesting data on the EV role in sexual transmission of Zika infection. They analyzed the effect of semen on ZIKV infection of cells and tissues derived from the anogenital region. In the presence of semen, infection by ZIKV and other flaviviruses was potently inhibited. They showed that semen prevented ZIKV attachment to target cells, and that extracellular vesicle was responsible for this anti-ZIKV activity. Their findings suggested that EVs and virions compete with same attachment factors on the surface of target cells. Thus, the high number of EVs in semen may outcompete Zika virions preventing sexual viral transmission.
Dr. Janis A. Müller discussed how human saliva affected ZIKV infectivity. They found that physiological concentrations of pooled saliva dose-dependently inhibited ZIKV infection of monkey and human cells by preventing viral attachment to target cells. The anti-ZIKV activity was saliva was not be abrogated by boiling, suggesting the antiviral factor was not a protein. Instead, they found that purified extracellular vesicles (EVs) from saliva inhibited ZIKV infection. Salivary EVs (saEVs) expressed typical EV markers and prevented ZIKV attachment to and infection of target cells at concentrations that were naturally present in saliva. The anti-ZIKV activity of saliva was conserved but the magnitude of inhibition varied between individual donors. Their findings provided a plausible explanation for why ZIKV transmission via saliva, i.e. by deep kissing have not been recorded and establish a novel oral innate immune defense mechanism against viral pathogens.
Dr. Gurudutt N. Pendyala highlighted recent research surrounding the impact of maternal immune activation (MIA), as well as the potential etiological role of EVs, in ZIKA-induced neurodevelopmental deficits in exposed offspring. Preliminary data from these studies revealed that MIA offspring demonstrated a higher inflammatory state in their brains beginning at birth, which subsequently led to impaired synaptogenesis. In addition, the increased inflammatory state also led to enhanced brain derived extracellular vesicles (BDE) size in the MIA offspring. Furthermore, analysis of RNA sequencing data identified distinct brain-derived extracellular vesicles (BDEs) miRNAs responsible for regulating key functional pathways associated with brain development that are more impacted in MIA offspring. Overall, these studies demonstrated that maternal immunity in response to ZIKV infection during pregnancy plays a significant role in impacting the neurological outcomes in exposed offspring.
Sara York presented research from the laboratory of Dr. David Meckes at FSU College of Medicine. The primary aim of this research was to assess how EVs are modified by Zika infection and to investigate the role of tetraspanin EV biogenesis proteins in Zika infection. Here, it was found that Zika infection resulted in a massive increase in EV numbers which exhibited altered sizes and densities, and that the Zika virus-modified EVs were capable of infecting cell types important to pathogenesis and spread in humans. Moreover, during infection endogenous CD63 was recruited to the core of the viroplasm, and Zika capsid presence and localization was modified depending upon cellular CD63 levels. These results suggested that the EV enriched tetraspanin CD63 regulates the release of EVs and Zika viral genomes and capsids following infection, thereby highlighting a potentially novel mechanism of Zika virus transmission and demonstrating the role of EV biogenesis and trafficking proteins in the modulation of Zika infection.
Dr. Siddappa N. Byrareddy from the University of Nebraska Medical Center presented on the topic “Role of Glycans and Extracellular Vesicles in Modulating Host-Virus Interaction of Zika Virus.” In his presentation, he shared data showing that ZIKV uses envelope (E) glycoprotein to interact with host cell receptors to facilitate entry. He also presented analysis of ZIKV E of various strains derived from different cells and found that these proteins were extensively modified with oligomannose, hybrid and complex N-glycans of a highly heterogeneous nature. Further, host cell surface glycans were found to strongly correlate with the glycomic features of ZIKV E. He also provided evidence that ZIKV affects the number, but not the size, of EVs isolated from placental cells. Subsequent miRNA analysis revealed differential expression and GO analysis identified metabolic processing, intracellular signal transduction, MAP signaling, calcium signaling, and chemokine signaling pathways, collectively suggesting significant alterations in the key brain development functions.
Dr. Rüdiger Groß followed up on thier previous work on seminal EVs to potently inhibit infection of flaviviruses such as Zika and Dengue virus in vitro. They now have purified the EVs from large volumes of complex source fluids using a combined tangential flow filtration and bind-elute size exclusion chromatography (TFF/BE-SEC) to isolate EVs from seminal plasma, saliva and vaginal lavage. Nanoparticle tracking analysis and transmission electron microscopy revealed a mean diameter of 180-190 nm for EVs isolated from saliva and vaginal lavage, while seminal plasma-derived EVs were slightly smaller (~ 140 nm diameter). Also, saliva-derived EVs contained high levels of CD14, an LPS-binding protein with proposed function in oral immunity, while it was undetectable on EVs purified from semen and vaginal lavage. Finally, EVs purified from all three sources dose-dependently inhibited infection of Zika virus (MR766) as well as HIV-1 (R5-tropic NL4-3) in vitro, although salivary and vaginal lavage EVs were more potent than seminal EVs. These findings may further explain the (lack of) transmission by certain viruses in routes involving these body fluids and guide new therapeutic strategies.
There was also a session devoted to HIV associated neurocognitive impairment, commonly referred to as NeuroHIV. Dr. Shilpa Buch discussed some of her latest findings on HIV Tat and Morphine-mediated impairment of blood brain barrier. She discussed how synaptodendritic injury and impairment of glial function have emerged as important phenotypes and correlates of NeuroHIV. In the presence of cART, Tat protein is still present in the brain of the treated patients and adding fuel to the fire is the co-morbidity of drug abuse in those infected with HIV-1 (i.e., opioids). Here they showed data that exposure of astrocytes to HIV Tat resulted in increased expression & release of several miRNAs in the EV cargo, specifically the brain-enriched miR-7, which upon uptake by the hippocampal neurons, resulted in loss of inhibitory synapses via downregulation of neuroligin 2 (NLGN2) -a known key regulator of inhibitory synapses. Exposure to morphine resulted in induction and release of miR-138 in the ADEVs, which in turn, were taken up the microglia, resulting in microglial activation, via binding to the endosomal toll like receptor TLR-7. Overall, they concluded that HIV Tat and morphine-ADEVs together can result in neuronal injury, impaired microglial activation and phatocytosis and induce brain pericyte migration and blood-brain barrier breach, thus adding to the neuroinflammatory burden of NeuroHIV.
Dr. Sowmya Yelamanchili also discussed role of Methamphetamine (Meth) in HIV-associated neurocognitive disorders (HAND). Meth and related amphetamine compounds, which are potent psychostimulants, are among the most commonly used illicit drugs. They found that EV released from HIV infected and Meth treated monocyte-derived macrophages (MDMs) enhanced syncytia formation and HIV pathogenesis in macrophages. Her lab isolated EVs from three groups of HIV infected MDMs treated either with Meth or cART or with both and treated cells with these EVs. Using immunohistochemistry and confocal imaging they found that the EVs released from Meth treated MDMs enhance syncytia formation and multinucleated cells. Western blot analysis revealed that ICAM1 was released in EVs and Meth enhanced their release. They concluded that Meth exposure enhanced syncytia formation, HIV pathogenesis, and toxicity in HIV infected cells.
Dr. Guoku Hu showed how astrocytes exposed to morphine and HIV Tat, can be taken up by neurons, leading to neuronal damage. They also identified the role of EVs and their cargo in the development of drug tolerance and addiction through the mechanism of sonic hedgehog (SHH) protein in morphine stimulated astrocyte-derived EVs. Furthermore, SHH containing morphine-ADEVs activated the SHH signaling in astrocytes both in vitro and in astrocytes of morphine-administered mice. Importantly, inhibition of EV release or primary cilia prevented morphine tolerance in C57BL/6 mice, concluding that an autocrine mechanism for SHH pathway activation in astrocytes could be associated with morphine tolerance.
Dr. Susmita Sil shared research investigating the role of astrocyte-derived EVs in neuronal injury and the role of HIF-1α-lncRNA BACE-1AS axis in HIV-1-associated neurocognitive disorders (HAND). Previous research from this laboratory has identified a role of HIF-1α-lncRNA BACE-1AS axis in HIV1-Tat mediated upregulation of toxic amyloid forms in astrocytes. Since HIF-1α is an upstream regulator of Tat-mediated amyloid production, it was hypothesized that blocking HIF-1α could mitigate neuronal injury. The uptake of Tat-stimulated astrocyte derived EVs (ADEVs) by neurons was assessed, as well as the extent of synaptic impairment. Rat hippocampal neurons exposed to Tat-ADEVs carrying toxic amyloids exhibited reduced dendritic spines and excitatory synaptic protein-PSD95, with a concomitant increase of the inhibitory synaptic protein- Gephryn. Furthermore, silencing of astrocytic HIF-1α not only reduced the release of ADEVs and their amyloid cargos, but also ameliorated neuronal injury. Thus, these studies have demonstrated the role of toxic amyloid cargo in ADEVs which have the potential to lead to neuronal injury and synaptic alterations.
The topic of HIV-1 associated drug addiction was further discussed by Dr. Norman Haughey from Johns Hopkins University School of Medicine. Although the precise mechanism for this enhanced susceptibility to drug addiction is unknown, there is evidence that chronic inflammation is associated with an increased sensitivity to addiction. However, the mechanism by which inflammation may contribute to addictive behavior has been elusive. Here, a role for EVs in mediating the cross talk between inflammation and the morphine addiction pathway was explored. Primary rat astrocytes stimulated with IL-1β released EVs containing 131 distinct miRNAs, with 10 increased and 17 decreased. Interrogation of the 17 decreased miRNAs found that miR-106b, miR-218a and miR-328a mapped to the morphine addiction pathway and bioinformatic analyses predicted these three miRNAs to target multiple genes in the morphine addiction pathway. Two of these miRNA targets were validated in HEK293T cells co-transfected with OPRM1-3′-UTR or KCNJ3-3’-UTR luciferase reporter vectors, and mimics for miR-218a and miR-328a, or a scrambled microRNA mimic. In cortical neurons exposed to a dose-response of EVs it was found that OPRM1, KCNJ3, DRD1 and GABBR2 mRNA and protein levels were increased in cells exposed to ADEV-IL-1β compared with ADEV-CR. These findings suggested that ADEV-CR carry miRNAs that chronically suppress the expression of key proteins in neural circuits associated with addiction and that modification of miRNA cargo in ADEV-IL-1β releases this chronic suppression and enhances activity of neural circuits responsive to opiates.
In another presentation, Dr. Eva Poveda emphasized the importance of identifying drivers of persistent immune activation and inflammation, such as EVs and mtDNA (a danger-associated molecule pattern-DAMP), in the absence of HIV replication. Data from a study designed to evaluate the profile of a specific subset of plasma EVs expressing CD9 from well-characterized cohorts of HIV-infected patients with different immunologic and virologic statuses as well as plasma from a control group of HIV-uninfected subjects was presented. The results demonstrated a massive increase of platelet-derived EVs among HIV-infected patients. Moreover, analysis of mitochondria and circulating cell-free mtDNA confirmed presence of mitochondria in EVs and revealed higher levels of circulating cell-free mitochondrial DNA (ccf-mtDNA) among HIV-infected patients that correlated to total EV numbers.
Dr. Susanne Gabrielsson presented data from ongoing studies using dendritic cell-derived exosomes to induce antigen-specific immune responses with an overall aim to cure cancer. Data from these studies have suggested that exosomes need to carry whole protein, and not only peptide/MHC complexes, to induce a strong T cell response in vivo and, moreover, that B-cell activation was required to induce a strong T cell response to exosomes. Testing of allogeneic exosomes in a B16 melanoma model demonstrated that allogeneic exosomes are as efficient in inducing immune responses as syngeneic exosomes. Additionally, loading exosomes with the CD1d ligand alpha-galactosyl ceramide, which stimulates NKT cells to produce interferon-gamma, further boosted antigen-specific T and B cell responses. These results highlight the potential of exosomes from antigen presenting cells as potential cancer immunotherapy vehicles.
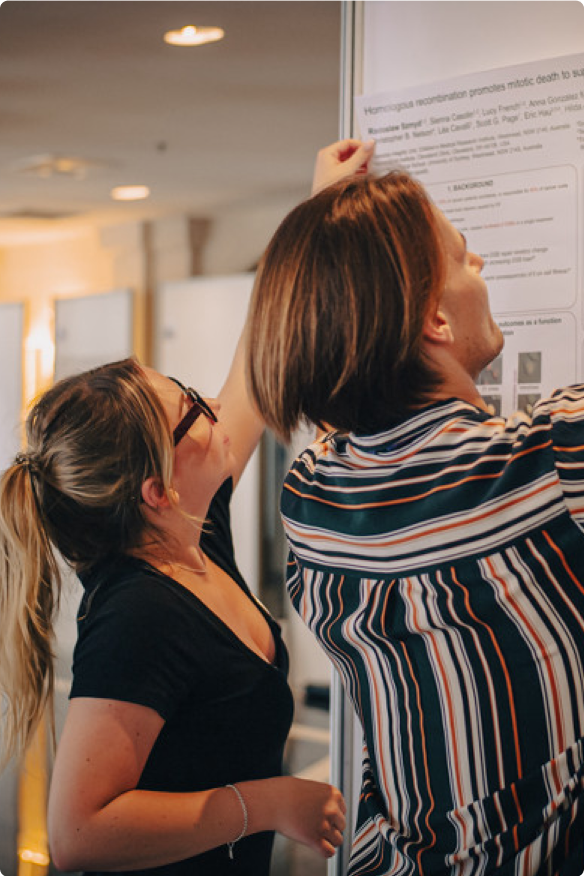
The meeting had one more critical event that included a mock-panel exercise of how to write a specific Aim page for NIH and other granting agencies. This session was open to all participants and generated a highly intellectual environment of sharing relevant ideas on grant writing related to Extracellular vesicles and infections.
We were very happy to welcome Nazar Filonov from Particle Metrix and thank him for Particle Metrix’s contribution as a Silver Sponsor at the meeting.
Thanks to the generosity of Steve Gould from ASEMV (American Society for Exosomes and Microvesicles) we also had the opportunity to award 3 x $250 short talk awards to junior investigators whose presentations and contributions to the meetings stood out. Congratulations to Monica Abou Harb (Florida State University), Rüdiger Groß (Ulm University Medical Centre) and Maria Kalamvoki (University of Kanas Medical Centre) for winning these awards.
The meeting was organized by Fusion over a six month period. They have done a superb job in communicating the relevant information to the organizers, the participants and worked tirelessly on the logistics. They were also generous with funding of the student and principal investigator travels as well as registration packages. During the meeting, our contact organizer (Ms. Amy Johnson) was attentive and managed to adjust the meeting schedules up to the day of the meeting. The logistics of room and board as well as the meals were superb. The meeting location was fantastic, as many of the participants continually complimented the science venue, the all-inclusive hotel environment and the beautiful Bahamas. Finally, as the meeting ended as the COVID-19 pandemic started, the Fusion organizers were careful and attentive to the needs of participants as they were leaving. Finally, I highly recommend working with Fusion to organize top rated scientific meetings which is in par with Gordon conferences in the United States.
Synopsis
Extracellular vesicles (EVs), which are generated by almost all living cells, are now considered to be an important system of cell–cell communication. A large volume of data has been published on EVs in different fields of biology and medicine, from immunology to marine biology. These data are discussed at large international meetings that gather thousands of researchers.
However, there is still a need for more-focused meetings at which the importance and reliability of the data should be evaluated by a narrow circle of experts. Here, we propose to organize a small conference that will focus on one of the most important aspects of EVs, their role in infectious human diseases. The aim of the proposed conference is to improve our understanding of the mechanisms of this involvement and to evaluate EVs as potential therapeutic targets.
Key Sessions to include:
- Extracellular vesicles generated by human cells: a diverse population of vesicles formed by diverse biogenesis and having diverse composition.
- Extracellular vesicles as mediators of communications between human cells in vitro and in vivo: proved cases vs. unproved hypotheses.
- Extracellular vesicles in retroviral pathogenesis: human retroviruses as close relatives of extracellular vesicles.
- Extracellular vesicles as carriers of viral proteins and infectious viruses.
- Extracellular vesicles in bacterial pathogenesis: effects of bacterial vesicles on human tissues.
- Extracellular vesicles in complicated pregnancies: EVs as mediators of disruption of mother-to-child dialogue in infections.
- Extracellular vesicles as vehicles carrying RNA and soluble factors between cells.
- Isolation and characterization of different vesicles generated by human cells in vivo and in vitro: Is this mission possible?
Student Offer
Take advantage of this fantastic opportunity for students! Register an academic at the earlybird rate and bring a student for only $850. Unfortunately, Postdocs are not eligible. Both registration packages include; accommodation for the 5,6,7 th March 2020 (on a shared basis for students) and a 24hour all-inclusive food and beverage package for the conference period. Academic registrations must be completed by 19th December 2019. Once registered, please contact Amy Johnson to obtain a special registration link for your student.
Confirmed Keynote Speaker
Yoel Sadovsky (Magee-Womens Research Institute)
PLACENTAL EXOSOMES IN VIRAL RESISTANCE AND FETAL-MATERNAL COMMUNICATION
Confirmed Plenary Speakers
Genoveffa Franchini (NIH)
RISK OF SIVmac251 ACQUISITION IN MACAQUES AND EXTRACELLULAR VESICLE MIRNAS ELICITED BY HIV VACCINE CANDIDATES
Stephen Gould (Johns Hopkins University)
MECHANISMS OF PROTEIN AND VIRUS BUDDING
Clotilde Thery (Institute Curie)
HETEROGENEITY OF EXTRACELLULAR VESICLES: WAYS OF DEFINING EV SUBTYPES
Guillaume van Niel (INSERM)
LIVE TRACKING OF EXOSOMES IN VIVO
Philip Stahl (Washington University in St. Louis)
Confirmed Invited Speakers
Igor Almeida (University of Texas)
ALPHA-GAL-CONTAINING EXTRACELLULAR VESICLES FROM TRYPANOSOMA CRUZI AS BIOMARKERS OF CHAGAS DISEASE
Shilpa Buch (Nebraska Medical Center)
Michael Bukrinsky (District of Columbia Center)
EXTRACELLULAR VESICLES CARRYING HIV NEF ARE THE KEY PLAYERS IN PATHOGENESIS OF HIV-ASSOCIATED CO-MORBIDITIES
Hernando Del Portillo (Barcelona Insititute for Global Health)
CIRCULATING PLASMA VESICLES FROM MALARIA PATIENTS FACILITATE PARASITE SEQUESTRATION IN THE HUMAN SPLEEN
Dirk Dittmer (UNC Lineberger)
FUNCTION OF EXOSOMES IN VIRAL LYMPHOMA
Susanne Gabrielsson (Karolinska University)
EXOSOMES IN LUNG DISEASES; ASTHMA, SARCOIDOSIS AND COPD.
Ramin Hakami (George Mason University)
MECHANISMS OF INNATE IMMUNE REGULATION BY EXOSOMES RELEASED DURING GRAM-NEGATIVE BACTERIAL INFECTIONS
David Meckes (Florida State University)
MODULATION OF HOST CELL EXTRACELLULAR VESICLE CARGO AND FUNCTIONS DURING VIRAL INFECTION
Jan Münch (Ulm University)
EVS IN SEMEN PREVENT ZIKV INFECTION – A NOVEL ANTIVIRAL INNATE IMMUNE DEFENSE MECHANISM?
Esther Nolte-'t Hoen (Universiteit Utrecht)
PATHWAYS UNDERLYING THE RELEASE OF PICORNAVIRUSES INSIDE SUBPOPULATIONS OF EXTRACELLULAR VESICLES
Rogers Palomino (NIH)
VAGINAL LACTOBACILLUS-DERIVED EXTRACELLULAR VESICLES IN PROTECTING FROM HIV-1 TRANSMISSION
Eva Povedra (Galicia Sur Health Research Institute)
EXTRACELLULAR VESICLES AND MITOCHONDRIAL DNA, NEW BIOMARKERS OF HIV PATHOGENESIS?
Ratna Ray (Doisy Research Center)
COMMUNICATION AMONG HCV INFECTED HEPATOCYTES AND OTHER LIVER CELLS VIA EXOSOMES
Hermann Schatzl (University of Calgary)
AUTOPHAGY AND EXOSOMAL RELEASE OF PRIONS
Yong Song Gho (Postech)
BACTERIAL EXOSOMES AS NEXT-GENERATION CANCER IMMUNOTHERAPY
Target Audience
The specific audience that will attend this conference will consist of the leading experts in extracellular vesicles, post-doctoral fellows, and possibly PhD students who plan to investigate the relevance and involvement of extracellular vesicles in their scientific projects, as well as physicians who have read about extracellular vesicle involvement in human diseases and who want to learn about this topic from the experts. The field of extracellular vesicles is relatively new, and the ideas so far developed are rather simple. Therefore, to understand the field at this stage of its development does not require prior knowledge or skills beyond general university courses in microbiology.
Educational Need
The field of extracellular vesicles has undergone extensive growth over the last several years; it has attracted significant funding and a diverse circle of researchers. As the result, the field benefits from excellent new data but is also held back by less-than-convincing results and unproved hypotheses. A relatively small conference focused on only one aspect of extracellular vesicles, namely their role in human infectious disease, may provide for the scientific community a consensus view of the leading experts on the validity of different data and may develop new lines of research necessary for the progress of basic knowledge of EVs and their potentials in translational medicine.
International Women's Day
International Women's Day is a global day celebrating the social, economic, cultural and political achievements of women across the world. The day also marks a call to action for accelerating gender parity. To mark the day we aim to dedicate the programme to an all-female speaker line up on Sunday 08 March 2020.
Confirmed Speakers
Plenary Speakers

Guillaume van Niel
research director, team leader, Institut de Psychiatrie et Neurosciences de Paris, INSERM U1266

Clotilde Théry
PI, Institut Curie/INSERMU932

Yoel Sadovsky
Executive Director, Magee-Womens Research Institute

Stephen Gould
Professor, Johns Hopkins University
Invited Speakers

SHILPA BUCH
Professor, University of Nebraska Med Ctr
Michael Bukrinsky
Professor, George Washington University

Jan Münch
Director, Ulm University Medical Center

Ramin Hakami
Associate Professor, George Mason University

Dirk Dittmer
Professor, University of North Carolina at Chapel Hill

Hermann Schatzl
Professor and Associate Dean, University of Calgary

Rogers Alberto Nahui Palomino
Post. Doc, National Institutes of Health

Eva Poveda
Research Group Leader, Group of Virology and Pathogenesis, Galicia Sur Health Research Institute

Susanne Gabrielsson
Professor, Karolinska Institutet

Esther Nolte-'t Hoen
Assistant Professor, Utrecht University

Steven Jacobson
Principal Investigator, National Institutes of Health
Programme
THURSDAY 5TH MARCH 2020 |
||
|
14:15 – 14:45 |
Registration & Welcome Reception |
|
|
Past and Future of EV Studies |
||
|
14:45 – 15:00 |
Opening Comments |
|
|
15:00 – 15:35 |
Yoel Sadovsky |
PLACENTAL EXOSOMES IN VIRAL RESISTANCE AND FETAL-MATERNAL COMMUNICATION |
|
15:35 – 16:10 |
Clotilde Thery |
HETEROGENEITY OF EXTRACELLULAR VESICLES: WAYS OF DEFINING EV SUBTYPES |
|
16:10 – 16:35 |
Herman Schatzl |
AUTOPHAGY AND EXOSOMAL RELEASE OF PRIONS |
|
16:35 – 17:10 |
Guillaume van Niel |
LIVE TRACKING OF EXOSOMES IN VIVO |
|
17:10 – 17:55 |
Refreshments |
|
|
EVs and ZIKA Infections |
||
|
17:55 – 18:10 |
Ruediger Gross |
ISOLATION AND CHARACTERIZATION OF ANTIVIRAL EXTRACELLULAR VESICLES FROM HUMAN BODY FLUIDS |
|
18:10 – 18:35 |
Jan Münch |
EVS IN SALIVA AND SEMEN PREVENT ZIKV INFECTION – A NOVEL ANTIVIRAL INNATE IMMUNE DEFENSE MECHANISM? |
|
18:35 – 18:50 |
Janis Muller |
SALIVARY EXTRACELLULAR VESICLES INHIBIT ZIKA VIRUS INFECTION |
|
18:50 – 19:05 |
Gurudutt Pendyala |
STRATEGIES TO R(EV)EAL THE ROLE OF MATERNAL IMMUNITY IN ZIKA INDUCED NEURODEVELOPMENTAL DEFICITS IN EXPOSED OFFSPRING |
|
19:05 – 19:20 |
Sara York |
ZIKA VIRUS HIJACKS EXTRACELLULAR VESICLE TETRASPANIN PATHWAYS FOR CELL-TO-CELL TRANSMISSION |
|
19:20 – 19:35 |
Siddappa Byrareddy |
ROLE OF GLYCANS AND EXTRACELLULAR VESICLES IN MODULATING HOST-VIRUS INTERACTION OF ZIKA VIRUS |
|
19:35 – 20:05 |
Discussion |
|
|
20:05 |
Dinner |
|
FRIDAY 6TH MARCH 2020 |
||
|
07:00 – 09:00 |
Buffet Breakfast at The Market Place |
|
|
EVs and Bacterial Infection |
||
|
09:00 – 09:25 |
Ramin Hakami |
MECHANISMS OF INNATE IMMUNE REGULATION BY EXOSOMES RELEASED DURING GRAM-NEGATIVE BACTERIAL INFECTIONS |
|
09:25 – 09:50 |
Rogers Palomino |
VAGINAL LACTOBACILLUS-DERIVED EXTRACELLULAR VESICLES IN PROTECTING FROM HIV-1 TRANSMISSION |
|
09:50 – 10:15 |
Michael Bukrinsky |
EXTRACELLULAR VESICLES CARRYING HIV NEF ARE THE KEY PLAYERS IN PATHOGENESIS OF HIV-ASSOCIATED CO-MORBIDITIES |
|
10:15 – 11:00 |
Group Photo & Refreshments |
|
|
11:00 – 11:15 |
Guoku Hu |
EVS IN HIV NEURODEGENERATIVE DISEASES |
|
11:15 – 11:40 |
Dirk Dittmer |
FUNCTION OF EXOSOMES IN VIRAL LYMPHOMA |
|
11:40 – 11:55 |
Dingani Nkosi |
EPSTEIN-BARR VIRUS LMP1 REORGANIZES THE CARGO AND FUNCTION OF EXTRACELLULAR VESICLES |
|
11:55 – 16:45 |
Lunch at Leisure & Free Time |
|
|
EV and Viruses |
||
|
16:45 – 17:10 |
Steve Jacobson |
EVS IN HTLV-1 |
|
17:10 – 17:35 |
Esther Nolte-t Hoen |
PATHWAYS UNDERLYING THE RELEASE OF PICORNAVIRUSES INSIDE SUBPOPULATIONS OF EXTRACELLULAR VESICLES |
|
17:35 – 17:50 |
Monica Abou Harb |
EPSTEIN-BARR VIRUS LMP1 REGULATES THE SECRETIONOF MICROVESICLE-ASSOCIATED PD-L1 |
|
17:50 – 18:05 |
Antonios Fikatas |
EXPLORING THE ROLE OF EXTRACELLULAR VESICLES ON THE HUMAN BLOOD-BRAIN BARRIER DURING ZIKA VIRUS INFECTION |
|
18:05 – 18:20 |
Catie DeMarino |
SIGNIFICANCE OF INFLAMMATORY EVS FROM ANTI-RETROVIRAL TREATED CELLS |
|
18:20 – 18:35 |
Susmita Sil |
ASTROCYTE DERIVED EXTRACELLULAR VESICLES IN NEURONAL INJURY: ROLE OF HIF-1α-lncRNA BACE1AS AXIS IN HAND |
|
18:35 – 18:50 |
Marwan E. El Sabban |
EXOSOMES DERIVED FROM ATL-CELLS ACTIVATE MESENCHYMAL STEM CELLS AND MODULATE LEUKEMIA PROGRESSION |
|
18:50 |
Dinner |
|
SATURDAY 7TH MARCH 2020 |
||
|
07:30 – 09:00 |
Buffet Breakfast at The Market Place |
|
|
EVs and Autophagy in Infections |
||
|
09:30 – 09:45 |
Maria Kalamvoki |
EVS IN HERPESVIRUS INFECTION |
|
09:45 – 10:00 |
Sowmya Yelamanchil University of Nebraska Medical School |
ROLE OF METHAMPHETAMINE INDUCED EXTRACELLULAR VESICLES IN HIV NEUROPATHOGENESIS AND TOXICITY |
|
EVs spread in Vivo |
||
|
10:00 – 10:25 |
Norman Haughey |
CHRONIC INFLAMMATION IN THE SETTING OF HIV INFECTION INCREASES THE EXPRESSION OF KEY PROTEINS REGULATING THE NEURAL CIRCUITRY OF ADDICTION THROUGH THE MODULATION OF ASTROCYTE DERIVED EXTRACELLULAR VESICLE MIRNA CARGO |
|
10:25 – 11:10 |
Part 1 - Writing a winning grant on EVs - Fatah Kashanchi |
|
|
11:10 – 16:30 |
Lunch at Leisure & Free Time |
|
|
EVs and Other Pathogens |
||
|
16:30 – 17:05 |
Stephen Gould |
MECHANISMS OF PROTEIN AND VIRUS BUDDING |
|
17:05 – 17:40 |
Fatah Kashanchi |
VIROSOMES: WHO COMES OUT FIRST? |
|
17:40 – 18:10 |
Refreshments |
|
|
Technical Advances for EV Analysis in Infectious Disease |
||
|
18:10 – 18:35 |
Anoop Pal |
DEVELOPMENT OF AN AUTOMATED, HIGH-PRECISION, STANDARDIZABLE EXTRACELLULAR VESICLE ISOLATION AND ANALYSIS PLATFORM FOR CLINICAL SAMPLES |
|
18:35 – 19:00 |
Nazar Filonov |
PARTICLE METRIX: NEXT GENERATION NANOPARTICLE TRACKING ANALYSIS |
|
19:00 – 19:25 |
Heather Branscome |
USE OF STEM CELL EXTRACELLULAR VESICLES AS A HOLISTIC APPROACH TOWARDS CNS REPAIR |
|
19:25 – 19:55 |
Part 2 - Writing a winning grant on EVs- Fatah Kashanchi |
|
|
20:00 |
Gala Dinner & Awards |
|
SUNDAY 8TH MARCH 2020 |
||
|
07:30 – 09:00 |
Buffet Breakfast at The Market Place |
|
|
EVs in Vaccination and Therapy of Infectious Diseases |
||
|
09:00 – 09:35 |
Genoveffa Franchini |
RISK OF SIVmac251 ACQUISITION IN MACAQUES AND EXTRACELLULAR VESICLE MIRNAS ELICITED BY HIV VACCINE CANDIDATES |
|
09:35 – 10:00 |
Susanne Gabrielsson |
EXOSOMES IN LUNG DISEASES; ASTHMA, SARCOIDOSIS AND COPD |
|
10:00 – 10:25 |
Shilpa Buch |
ROLE OF HIV1-Tat INDUCED ASTROCYTE DERIVED EXTRACELLULAR VESICLE MIRNAS IN DISRUPTION OF THE BLOOD-BRAIN BARRIER |
|
10:25 – 10:50 |
Eva Poveda |
EVS IN HIV-INFECTED PATIENTS |
|
10:50 – 11:15 |
‘Review of the Field’ by Clotilde Thery, Institute Curie |
|
|
11:15 – 11:30 |
Closing Comments |
|
Supported by
Venue & Location
Melia Nassau Beach All Inclusive
Overlooking one of the finest beaches in the world the Meliá Nassau Beach is surrounded by crystal blue waters and white sandy beaches. Located on the stunning Cable Beach, you are just a few minutes walk from the center, shops and restaurants. The beautiful Nassau Botanical Gardens are within easy reach (7km) and Lynden Pindling International Airport is situated only 9km away.
Throughout your stay delegates will enjoy a full meal plan, inclusive of beverages. Take your pick from Cilantro where you can experience the natural textures, aromas and flavors of Mexico, Nikkei, celebrated for its exquisite fusion of Japanese, Cantonese and Peruvian cuisine featuring a sushi bar and Teppanyaki tables, Estavida, an upbeat tapas lounge located in the hotel lobby serving innovative tapas and a wide selection of cocktails, Aqua, an A la carte restaurant specializing in exquisite, rustic Italian cuisine, The Market Place, where you will find an International buffet serving an array of exquisite dishes, O'Grille, an open air restaurant with fabulous views of the sea and pool serving casual beach fare and light bites and finally The Black Angus, a steakhouse featuring hip, contemporary jazz and modern decor, offering guests the finest quality prime cuts and the freshest ingredients.(This restaurant is not included in the all inclusive package, additional charges apply). The Gala Night takes place on the third evening of the conference with a mouth-watering feast of local cuisine, an open bar and amazing local entertainment. We welcome all delegates and their accompanying persons to the Gala Night – a truly fun filled night not to be missed!
Hotel Facilities
- 24 hour reception
- Room service
- 3 heated outdoor pools
- Complimentary resort wide Wi-Fi (guest rooms, throughout hotel, beach and conference areas)
- 24-hour Fitness Center
- 7 dining venues
- 4 bars.
- non-motorised water sports
The Bahamas is formed by over 700 islands, keys and islets located in the Atlantic Ocean and renowned for its warm sunshine, mild climate, fine, white sandy beaches, turquoise, crystal clear water and friendly people, making this the perfect environment to relax and unwind in your free time during the conference.
General Information
Venue Rating
★ ★ ★ ★
Currency
US Dollar (USD)
Address
Nassau W Bay St. Nassau Bahamas
Nearest Airport
Lynden Pindling International Airport
Location
The Melia Nassau Beach All-Inclusive is located right on the stunning Cable Beach just a few minutes away from the airport and city center; Nearby in Downtown Nassau you can experience the flavours of new foods at local restaurants, shop 'til you drop at Straw market or take a trip through time at the Pirates Museum. The beautiful Nassau Botanical Gardens are close by and water enthusiasts can enjoy non-motorized water sports right on property.
Nassau is the capital of the Bahamas. It lies on the island of New Providence, with neighboring Paradise Island accessible via Nassau Harbor bridges. The city has a hilly landscape and is known for it's fabulous beaches as well as its offshore coral reefs, popular for diving and snorkeling. It retains many of its typical pastel-colored British colonial buildings, like the pink-hued Government House.
If you are interested in this meeting but not yet ready to register, you can sign up for updates here and our team will keep you updated regarding deadline reminders and grant opportunities relating to this meeting only.
If you're interested in sponsoring this conference please contact us.
Conference Manager

Meredith Willmott

Need some help? Chat to the Fusion team today
As a family run business, our dedication runs deep. We’re committed to each other and, even more so, to every attendee’s experience, delivering a level of care and passion that’s truly unmatched.